To use all functions of this page, please activate cookies in your browser.
my.chemeurope.com
With an accout for my.chemeurope.com you can always see everything at a glance – and you can configure your own website and individual newsletter.
- My watch list
- My saved searches
- My saved topics
- My newsletter
Blood film
A blood film or peripheral blood smear is a slide made from a drop of blood, that allows the cells to be examined microscopically. Blood films are usually done to investigate hematological problems (disorders of the blood itself) and, occasionally, to look for parasites within the blood such as malaria and filaria. Product highlight
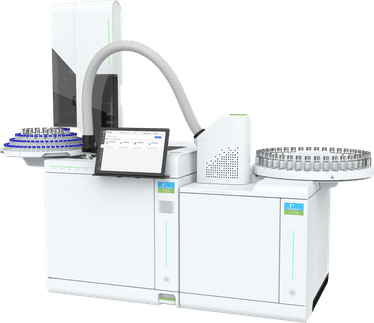
PreparationBlood films are made by placing a drop of blood on one end of a slide, and using a spreader slide to disperse the blood over the slide's length. The aim is to get a region where the cells are spaced far enough apart to be counted and differentiated. The slide is left to air dry, after which the blood is fixed to the slide by immersing it briefly in methanol. The fixative is essential for good staining and presentation of cellular detail. After fixation, the slide is stained to distinguish the cells from each other. Common blood film staining methods
InterpretationRoutine examinationA blood film will help identify circulating blood cells. Apart from counting the cells, morphology of cells can provide a wealth of information and assist in making a diagnosis.[1] Cellular components of blood are:
Normal blood films are typically full of red blood cells, with occasional white blood cells and minuscule platelets, which are harder to notice due to their size. DisordersCharacteristic red blood cell abnormalities are anemia, sickle cell anemia and spherocytosis. Sometimes the microscopic investigation of the red cells can be essential to the diagnosis of life-threatening disease (e.g. TTP). White blood cells are classified according to their propensity to stain with particular substances, the shape of the nuclei and the granular inclusions.
Use in diagnosing malariaThe preferred and most reliable diagnosis of malaria is microscopic examination of blood films, because each of the four major parasite species has distinguishing characteristics. Two sorts of blood film are traditionally used. Thin films are similar to usual blood films and allow species identification, because the parasite's appearance is best preserved in this preparation. Thick films allow the microscopist to screen a larger volume of blood and are about eleven times more sensitive than the thin film, so picking up low levels of infection is easier on the thick film, but the appearance of the parasite is much more distorted and therefore distinguishing between the different species can be much more difficult.[2] From the thick film, an experienced microscopist can detect parasite levels down to as low as 0.0000001%. Microscopic diagnosis can be difficult because the early trophozoites ("ring form") of all four species look identical and it is never possible to diagnose species on the basis of a single ring form; species identification is always based on several trophozoites. Please refer to the chapters on each parasite for their microscopic appearances: P. falciparum, P. vivax, P. ovale, P. malariae. The biggest pitfall in most laboratories in developed countries is leaving too great a delay between taking the blood sample and making the blood films. As blood cools to room temperature, male gametocytes will divide and release microgametes: these are long sinuous filamentous structures that can be mistaken for organisms such as Borrelia. If the blood is kept at warmer temperatures, schizonts will rupture and merozoites invading erythrocytes will mistakenly give the appearance of the accolé form of P. falciparum. If P. vivax or P. ovale is left for several hours in EDTA, the build up of acid in the sample will cause the parasitised erythrocytes to shrink and the parasite will roll up, simulating the appearance of P. malariae. This problem is made worse if anticoagulants such as heparin or citrate are used. The anticoagulant that causes the least problems is EDTA. Romanovski's stain or a variant stain is usually used. Some laboratories mistakenly use the same stain as they do for routine haematology blood films (pH 7.2): malaria blood films must be stained at pH 6.8, or Schüffner's dots and James's dots will not be seen. References |
|
| This article is licensed under the GNU Free Documentation License. It uses material from the Wikipedia article "Blood_film". A list of authors is available in Wikipedia. |