To use all functions of this page, please activate cookies in your browser.
my.chemeurope.com
With an accout for my.chemeurope.com you can always see everything at a glance – and you can configure your own website and individual newsletter.
- My watch list
- My saved searches
- My saved topics
- My newsletter
Cytochrome P450 reductaseCytochrome P450 reductase (EC 1.6.2.4; also known as NADPH:ferrihemoprotein oxidoreductase, NADPH:hemoprotein oxidoreductase, NADPH:P450 oxidoreductase, P450 reductase, CPR, POR)
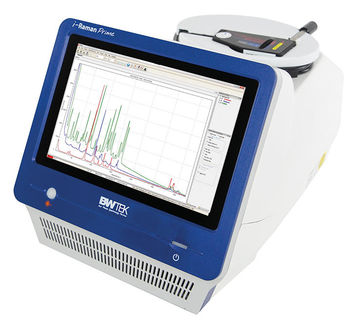
Product highlight
IntroductionEukaryotic microsomal cytochrome P450 enzymes and some bacterial P450s receive electrons from a FAD- and FMN-containing enzyme NADPH:cytochrome P450 reductase (CPR; EC 1.6.2.4). Microsomal CPR is membrane-bound protein that interacts with different P450s. In Bacillus megaterium and Bacillus subtilis, CPR is a C-terminal domain of CYP102, a single polypeptide self-sufficient soluble P450 system (P450 is an N-terminal domain). The general scheme of electron flow in the CPR/P450 system is:
The definitive evidence for the requirement of CPR in cytochrome-P450 mediated reactions came from the work of Lu, Junk and Coon [1], who dissected the P450-containing mixed function oxidase system into three constituent components: CPR, cytochrome P450 and lipids. Since all microsomal P450 enzymes require CPR for catalysis, it is expected that disruption of CPR would have devastating consequences. CPR knockout mice are embryonic lethal[2], probably due to lack of electron transport to extrahepatic P450 enzymes since liver-specific knockout of CPR yields phenotypically and reproductively normal mice that accumulate hepatic lipids and have remarkably diminished capacity of hepatic drug metabolism[3]. The reduction of cytochrome P450 is not the only physiological function of CPR. The final step of heme oxidation by mammalian heme oxygenase requires CPR and O2. In yeast, CPR affects the ferrireductase activity, probably transferring electrons to the flavocytochrome ferric reductase[4]. Gene organisationHuman CPR gene has 16 exons and the exons 2-16 code for a 677 amino acid [5] CPR protein (NCBI NP_000932.2). There is a single copy of 50 kb CPR gene (NCBI NM_000941.2) in humans on chromosome 7 (7q11.23). Mutations and polymorphismsFlück et al.[6] have reported for the first time five missense mutations (A284P, R454H, V489E, C566Y, and V605F) and a splicing mutation in the CPR genes of four patients who had hormonal evidence for combined deficiencies of two steroidogenic cytochrome P450 enzymes - P450c17 CYP17A1, which catalyzes steroid 17α-hydroxylation and 17,20 lyase reaction, and P450c21 21-Hydroxylase, which catalyzes steroid 21-hydroxylation. Later on Arlt et al.[7] identified another CPR missense mutation, Y178D, and also reported three of the CPR mutations (A284P, R454H, and C566Y), that were originally described by Flück et al.. In a larger study Huang et al.[8] have examined the CPR genes in 32 additional patients. Fifteen of nineteen patients having abnormal genitalia and disordered steroidogenesis were homozygous or apparent compound heterozygous for CPR mutations that destroyed or dramatically inhibited CPR activity. Huang et al. studied 11 new CPR variants: A115V, T142A, Q153R, P228L, M263V, R316W, G413S, Y459H, A503V, G504R, G539R, L565P, R616X, V631I, and F646del. CPR Deficiency – Mixed Oxidase DiseaseCPR deficiency is the newest form of congenital adrenal hyperplasia first described in 2004[6]. The index patient was a newborn 46,XX Japanese girl with craniosynostosis, hypertelorism, mid-face hypoplasia, radiohumeral synostosis, arachnodactyly and disordered steroidogenesis. However the clinical and biochemical characteristics of patients with CPR deficiency are long known in the literature as so-called mixed oxidase disease as CPR deficiency typically shows a steroid profile that suggests combined deficiencies of steroid 21-hydroxylase and 17α-hydroxylase/17,20 lyase activities. The clinical spectrum of CPR deficiency ranges from severely affected children with ambiguous genitalia, adrenal insufficiency and the Antley-Bixler skeletal malformation syndrome (ABS) to mildly affected individuals with polycystic ovary syndrome like features. Some of the CPR patients were born to mothers who became virilized during pregnancy, suggesting deficient placental aromatization of fetal androgens due to a lesion in microsomal aromatase resulting in low estrogen production. However, it has also been suggested that fetal and maternal virilization in CPR deficiency might be caused by increased dihydrotestosterone synthesis by the fetal gonad through an alternative "backdoor" pathway first described in the marsupials. Gas chromatography/mass spectroscopy analysis of urinary steroids from pregnant women carrying a CPR-deficient fetus supports the existence of this pathway[9], but the relevance of the "backdoor" pathway in the normal or CAH fetus remains unclear. The role of CPR mutations beyond CAH remains unknown; and questions such as how CPR mutations cause bony abnormalities and what role CPR variants play in drug metabolism by hepatic P450s are unsolved. However, reports of ABS in some offsprings of mothers who were treated with fluconazole, an antifungal agent which interferes with cholesterol biosynthesis at the level of CYP51 activity - indicate that disordered drug metabolism may result from deficient CPR activity. Structure3D crystal structure of rat CPR has been solved[10] (PDB 1AMO). The molecule is composed of four structural domains: the FMN-binding domain, the connecting domain, the FAD-binding domain and NADPH-binding domain. The FMN-binding domain is similar to the structure of FMN-containing protein flavodoxin, while the FAD-binding domain and NADPH-binding domains are similar to those of flavoprotein ferredoxin-NADP+ reductase (FNR). The connecting domain is situated between the flavodoxin-like and FNR-like domains. CPR homologsThe other enzymes containing homologs of CPR are nitric oxide synthase (EC 1.14.13.39), NADPH:sulfite reductase (EC 1.8.1.2), and methionine synthase reductase (EC 1.16.1.8). See alsoReferences
|
||||||||||||||||||||||||||||||||||||||||||||
| This article is licensed under the GNU Free Documentation License. It uses material from the Wikipedia article "Cytochrome_P450_reductase". A list of authors is available in Wikipedia. | ||||||||||||||||||||||||||||||||||||||||||||