|
|
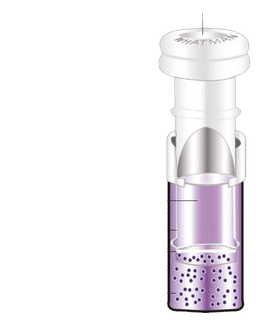
| DQ8 binding pocket with ligand PDB 1S9V [1]
|
| major histocompatibility complex, class II, DQ
|
| Haplotype(s)
| DQA1*0301:DQB1*0302, DQA1*0302:DQB1*0302
|
| Structure
|
| Type
| Cell surface receptor
|
| Quartenary
| αβ-heterodimer, ligand
|
| Ligand
| polypeptides, >9 residues DQ type restricted
|
| MMDB
| 17145
|
| Identifiers | alpha 1 *0301
|
| Symbol(s)
| HLA-DQA1 CELIAC1
|
| Entrez
| 3117
|
| OMIM
| 146880
|
| EBI-HLA
| DQA1*0301
|
| Identifiers | beta 1 *0302
|
| Symbol(s)
| HLA-DQB1
|
| Entrez
| 3119
|
| OMIM
| 604305
|
| EBI-HLA
| DQB1*030201
|
| Shared data
|
| Locus
| chr.6 6p21.31
|
HLA-DQ8 (DQ8) is an HLA-DQ serotype that recognizes the common HLA DRB1*0302 and the less common HLA DRB1*0304 gene products. DQ8 is a form of 'split antigen' of the broad antigen group DQ3 which also contains DQ7 and DQ9. DQA1*0301 : DQB1*0302 is the most common DQ8 type but other alpha (DQA1*0302, *0303, *0401 and *0503) and beta (DQB1*0304 and *0305) may be recognized as part of the DQ8 antigen.
Certain HLA-DQ isoforms are more commonly associated with certain autoimmune diseases. DQ8 stands out because of its association with juvenile diabetes, coeliac disease. It is also linked to HLA-DR alleles that are implicated in rheumatoid arthritis and may increase risk. HLA-DQ is not spread uniformly and certain populations are at increased risk; however that risk is often dependent on environment (e.g. Triticeae glutens consumption)
Serology
Serotyping efficiency.
DQ8, DQ3, and DQ7 recognition of Some DRB1*and [2]
| DQB1* | DQ8
| DQ3 | DQ7 | Sample
|
| allele | % | % | % | size (N)
|
| 0302 | 66 | 23 | 4 | 6687
|
| 0304 | 40 | 35 | 8 | 111
|
| 0305 | 34 | | 30 | 70
|
Haplotypes
DQ8.1 distribution
DQA1*0301:DQB1*0302 (DQ8.1) is the most common DQ8 subtype representing over 98% of the population. Infrequently DQA1*0302 is linked to DQB1*0302 but this substitution appears not to alter DQ8.1 function. DQ8.1 is found almost ubiquitously in every human regional population, but because of its unique distribution it becomes an object of molecular anthropology. There are 3 primary areas of haplotype elevation, Central and South America, NE Pacific Rim, and Northern Europe.
DQA1*03/DQB1*0302 levels in the Americas (given as frequency in %)
| | Reference
| DQA1
| DQB1
| Estimated
|
| | Population
| *03 | *0302
| DQ8.1
|
| [1]
| Lacandon (mayan)
| 79.0 | 77.9
| 77.9
|
| [3]
| Perija-Yucpa (Venezuela)
| 74.0 | 75.0
| 74.9
|
| [4][2]
| Mayan (Guatemala)
| | 48.1
| 47.6
|
| [5][3]
| Mazatecans (Mexico)
| 48.5 | 48.5
| 47.5
|
| [6] [4]
| Lamas (Peru)
| | 45.2
| 44.7
|
| [5]
| Dakota Sioux (S. Dakota)
| 52.1 | 45.0
| 44.5
|
| [7][6]
| Mixtec(Oaxaca, Mexico)
| 40.0 | 35.9
| 35.4
|
| [8][7]
| Lakota Sioux (S. Dakota)
| | 25.7
| 25.5
|
| [9][8]
| Terena (Brazil)
| | 17.5
| 17.0
|
| [9]
| Cauc., San Antonio (USA)
| | 11.7
| 11.7
|
| [10]
| Caucasian (USA)
| 18.5 | 10.5
| 10.5
|
| [11][10]
| African American (SE. USA)
| | 4.9
| 4.5
|
| [12]
| Tlinglet (Alaska, USA)
| 14.0 | 8.5
| 8.5
|
| [13][11]
| Eskimo (Alaska, USA)
| | 3.8
| 3.8
|
| [12]
| Canoncito Navajo (USA)
| 6.3 | 3.5
| 3.5
|
| [14]
| Eskimo (E. Greenland)
| 0.0 | 0.0
| 0.0
|
High Frequencies in the Americas
The global node for DQ8 is in Central America and northern South America where it reaches the highest frequency for any single DQ serotype, close to 90% phenotype frequency (77% haplotype frequency), and is at relatively high frequency in the indigenous North American population, and the coastal regions of the Gulf of Mexico and up the Mississippi Valley. The high freqeuncy of DQ8 in South America's northeastern regions[3] and low frequency in Indigenous Americans of more recent Asian ancestry [14][12] or Siberian origin[15] suggest that DQ8 was at high frequency in the earliest Amerinds. The pattern of distribution is consistent with recent mtDNA results suggesting the first migrants to the New World settled in the lowland coastal regions, river valleys and moved slowly inland, subsequent settlers moved into the highland regions. DQ8 and DQ2.5 have many analogous functional similarities, and this first settler bias may be a reason for the similarity. Studies on Epstein Barr Virus[16] and other proteins suggest both proteins are acidic (meaning peptides with increased negative charge) peptide presenters (see DQ8 for an illustration of the presentation process) and may have been adaptive for certain hunting and gathering lifestyles, possibly coastal foragers.
Abundance in Asia
DQA1*03/DQB1*0302 levels in the Asia (given as frequency in %)
| | Reference
| DQA1
| DQB1
| Estimated
|
| | Population
| *03 | *0302
| DQ8.1
|
| [15]
| Nivkhi (NNE. Sakalin I.)
| | 0.0
| 0
|
| [13][17]
| Zorastra, Yadz (Iran)
| 20.8 | 0.8
| 0.8
|
| [14][18]
| Khoton (Mongolia)
| 24.4 | 1.2
| 1.2
|
| [15]
| Madang (Papua New Guinea)
| 1.5 | 1.5
| 1.5
|
| [16][19]
| Yao (China)
| | 2.6
| 2.6
|
| [17][20]
| Naxi, Lijiang (China)
| | 2.7
| 2.7
|
| [21]
| Ainu (Japan)
| | 3.0
| 3.0
|
| [18][22]
| Shandong Han (China)
| | 3.1
| 3.1
|
| [18][23]
| Khalkha (Mongolia)[19][20]
| 22.3 | 6.1
| 6.1
|
| [21]
| Thais
| 21.5 | 7.4
| 7.4
|
| [22][24]
| Ket, Yenisey(Siberia)
| 14.7 | 8.4
| 8.4
|
| [25]
| South Korea
| | 10.3
| 10.3
|
| [26]
| Japanese
| | 10.8
| 10.8
|
| [23][24]
| Nganasan (siberia)
| 39.6 | 11.4
| 11.4
|
| [24][27]
| Uygars, Urumqi (China)
| 21.9 | 11.4
| 11.4
|
| [28]
| Kazahk
| | 11.4
| 11.4
|
| [25][29]
| Negidal (Siberia)
| 50.0 | 18.6
| 18.6
|
| [30]
| Cook Isl. (Pacific)
| | 25.0
| 25.0
|
Hiatus of DQ8 in the NE Siberian Arctic, Elevated Levels in Amur Region and Eastern Turks
The levels of DQ8 in SW to West Pacific Rim are at variable haplotype frequencies, from 2 to 30%, and level off around 10% for Ryūkyūan, Japanese, Koreans, Amur Regions and in the NW Pacific Rim drop to less than 1% in the Nivkhi. There is a modern hiatus of DQ8 in the Alaska-Eastern Siberian region and it is unclear whether this is due to replacement, selection, or the mode in which first Americans arrived (i.e strictly maritime route). The DR types associated
with DQ8 are DRB1*0403, *0404, *0406, *0407, *0408, and *0401 is split between many DQA1:B1 haplotypes. DQB1*0405 is commonly associated with DQA1*0303:DQB1*04 and so it is not included
in DRB1*0401 in high resolution assessments. The Cook Island DQ8 had only one associated
DR haplotype suggesting diversity limiting introduction into the region, either via
the TW-(Japan/Korea/China) route or through the west, for example the Bunun have high DRB1*0403. The majority of DRB1*04 appear to have redistributed from eastern Asia
from an unknown source, possibly in Central Asia or India. The distribution can be compared with Native Groups such as South Americans. Three groups with high levels, the Kogui, Sikuni, and Yucpa, have about 75% DQ8, the dominant DRB1* allele in 2 of 3 is the *0411 (N. China = 0), but *0407 (Ryūkyū, Japanese, Mansi-Eastern Ural, Naxi Chinese) and *0403 (Nganasan, Buryat, Negidal, Tunisians, Ryūkyū, Korea, Ainu) are also found. In North America DRB1*0404 and *0407 are more common than *0403 and, in the Lakota Souix, B1*0411 is rare. The DRB1*0404-DQ8 haplotype is more common in North Western Asia, and Northern Europe.
High Levels of DQ8 in Northern Europe
DQA1*03/DQB1*0302 levels in the Europe, Middle East and Africa (given as frequency in %)
| | Reference
| DQA1
| DQB1
| Estimated
|
| | Population
| *03 | *0302
| DQ8.1
|
| [26][31]
| Nenets (N. Russia)
| 40.9 | 20.9
| 20.0
|
| [27][31]
| Murmansk Saomi (Russia)
| 38.3 | 18.5
| 17.2
|
| [28][32]
| Gaza (Israel/Palestine)
| | 17.6
| 17.0
|
| [29][31]
| Arkhange Pomors(Russia)
| 22.6 | 17.1
| 16.4
|
| [30][33]
| Swedish
| 24.2 | 18.7
| 16.1
|
| [31][34]
| Caucasian (England)
| 23.7 | 16.4
| 15.9
|
| [32][35]
| Finland
| | 15.7
| 15.2
|
| [36]
| France's CEPH
| 21.3 | 14.5
| 13.5
|
| [33][33]
| Dane
| 20.9 | 13.2
| 13.2
|
| [37]
| Dutch
| | 11.2
| 11.0
|
|
| Irish
| |
| 10.6
|
| [34][38]
| NW Slavic (Russia)
| 16.0 | 11.0
| 10.5
|
| [33]
| German
| | 10.5
| 9.9
|
| [31]
| Russian
| | 8.9
| 7.2
|
| [39]
| Cantabarian (Spain)
| 19.3 | 8.4
| 7.0
|
| [33]
| Spanish
| | 8.9
| 6.5
|
| [33]
| Sardinian
| | 4.9
| 4.9
|
| [33]
| Italian
| | 4.6
| 4.5
|
| [40]
| United Arab Emirates
| | 0.83
| 0.8
|
| [41]
| Jordon
| 24.1 | 17.9
| 17.9
|
| Africa
|
| [33]
| !kung
| | 36.7
| 36.7
|
| [33]
| Khoi
| | 14.9
| 13.9
|
| [42]
| Oromo
| 17.5 | 9.0
| 9.0
|
| [43]
| Morocco
| 17.2 | 8.9
| 8.6
|
| [44]
| Tunisia
| 10.31 | 10.0
| 8.0
|
| [42]
| Amhara
| 11.2 | 5.6
| 5.6
|
| [45]
| Aka pygmies
| | 3.2
| 3.0
|
| [33]
| Negroid (N. Africa)
| | 3.1
| 2.7
|
| [46]
| Cameron
| 11.5 | 1.5
| 1.2
|
| [45]
| Bantu Congo
| | 0.6
| 0.5
|
| [47]
| Gabonese
| 7.5 |
| 0.5
|
| [48]
| Bubi
| 17.5 | 0.0
| 0.0
|
DQ8 is also abundant also in Northern Europe and is found at high frequencies in the German-Scandinavian-Uralic population north of Switzerland. HLA A-B haplotypes suggest that a migration from people east of the Urals is responsible for DQ8, possibly from as far east as the West Pacific Rim. The high level of DQ8 and DQ2.5 is something of great interest for DQ mediated diseases of Scandinavia and Northern Europe. DQ8 is also found in Iberia and places were east to west gene flow by other genetic markers cannot be substantiated, and the levels within the African or middle eastern population are possible sources, Iberia has considerable A1/B1 equilbration suggesting independent sources from Africa.
Other DQ haplotypes
DQA1*0503:DQB1*0302 (Mexico) and DQA1*0401:DQB1*0401 Siberia are two other DQ8 haplotypes that are rarely found.
Global Spread of DQ8
DQ8 along with a few other Haplotypes appears to be split NW/SE in Eurasia and with the evidence for DQ2.5 and other haplotypes suggest an ancient Central Asian population was displaced by a more recent African migration. There are many common markers found in France, Germans, Danes, Swedes, Tibetians, Amur River, Japanese and Koreans that are potential indicators of this bilateral spread. The DQ8 haplotypes is found at high frequencies in the !kung, albeit one expects more DQ8 in Austronesia it is ubiquitously spread if at some times low frequencies, other times higher frequencies (Thai). The path of DQ8 spread to the New World is enigmatic, certainly Japan and Amur River are potent sources, but other displaced populations cannot be ruled out. If the mode of travel was through the Beringia corridor as proposed by archaeologist, the very low frequency of DQ8 at present is a very unusual find with regard to evidence for complete displacement elsewhere in the World. Markers
that are shared between Japanese, TW-aboriginals tend to decline in frequency as one approaches Siberia, mtDNA markers decline in the Kuril chain. During the Jōmon period of Japan it appears
there would have been displacement by Ninhvet/Ainu ancestors and depression of DQ8 through out northern Japan, but the decline throughout the region is somewhat inexplicable outside of a catastrophic climate event between the settling of the New World and the current time.
An alternative model is that there were multiple sources of DQ8 in the peopling of NE Asia, some sources were from central Asia and some from the indochinese region, some of the DQ8 found in NW eurasia could be from an admixture of West pacific Rim and Central Asian sources, and were displaced from the more central regions but not from the more Eastern regions.
DQ8 and Selection
Like DQ2.5, DQ8 might have been under selection for maritime, coastal foraging peoples and in particular for peoples adapted to the climate/habitat situation on the northern end of the habitable west pacific rim at the Last Glacial Maximum. Triticeae cultivation may apply negative selection on DQ8. While there were numerous members of Triticeae species similar to Mid Eastern wild Triticeae in the Americas, and a great number of domesticated plants in the new world, no single species of Triticeae appears to have been domesticated in the New World, and no clear examples in closely related tribes of grasses. Among new world grass species in post Columbian times, one species of Elymus has been domesticated for human consumption and another as a pastoral cultivar. This could be interpreted in 2 ways. First, that levels of DQ8, negatively, inhibited the domestication of Triticeae strains. Second, that the absence of such cultivars more suitable than already developed cultivars allowed DQ8 to rise or remain high, while DQ2.5 levels in NW under much longer term selection have fallen, or a little of both. Most of American cultivars were domesticated south of the Rio Grande river (exceptions are Caddo rice and Texas varigated squash, etc.). Wheat, particularly Barley and Rye are preferential cultivars in cooler climate, whereas Zea is more adaptive in tropical climates and some cultivars are relatively drought tolerant, Zea however lacks certain amino acids that must be supplimented by other foods to prevent malnutrition. The proximity of neolithization to the Equator in the New World may have much to do with the unapparent negative selection of DQ8 relative to the neolithization of Western Eurasia.
DQ8 and Disease
In the United States, however there appears to be shift in autoimmune disease risk for immigrants from Mexico. Increased immunoreactivity of Hispanics in Houston appear to be associated with DQ8 and not DQ2.5. One of the issues is whether Triticeae and other dietary shifts are involved, or, to rephrase, the tissue transglutaminase reactivity of Zea is low, but high towards triticeae, milk proteins and meat collagen. Each of these has increased in the post-Columbian diet. So that there is at least the potential that damaging factors to the intestines couple with Zea-diet-adapted immune system explains the rise of a percentage diabetes and other autoimmune disease in Hispanics living in the United States.
In Japan DQ3 (DQ7, DQ8, DQ9) is associated with Myasthenia gravis in the early onset female population, though it does not appear DQ8 has the greater role, there are similarities between myastenia gravis in Japan and that detected in the Houston hispanic population, with DQ8 associated with younger females relative to the associations of all other HLA DQ types. Coeliac Disease is on the rise in Japan, and it is clear that dietary shifts are the reason, but, also there is no DQ2.5 in Japan and therefore it is not a risk factor. Diabetes, which was once considered a problem of the wealthy in Japan, but is also on the rise in the general population. The similarities with the Indigeonous Americans cannot be dismissed, because both wheat consumption, beef consumption and milk consumption are on the rise in Japan, but since there is no DQ2.5 the increased risk of late onset and Type I/II is almost eliminated from consideration.
In Europe, DQ8 is associated with Coeliac Disease and Type 1 diabetes has been well
established, however since DQ8 is less common than DQ2.5 and since DQ2.5 presents
more alpha-gliadin peptides it is more often attributed to Coeliac Disease. Since both
DQ2.5 and DQ8 are high in Scandinavia the problem is exaccerbated by enhanced susceptibility
of heterozygotes which also applies to increased frequencies of late onset Type I and ambiguous Type I/II diabetes. DQ8 is also found in many indigeonous peoples of Asia, it was detected early on in the Bedoin population of Arabia where DQ2.5 is frequently absent, and in these instances DQ8 is solely associated HLA in Coeliac Disease.
The DR4 linkage
Many disease associated with DQ8 have dual linkage with DR4, and certain DR4 (*0405) have
independent and dependent risk association with DQ8, for example with Juvenile diabetes[49][50].
References
- ^ Lee K, Wucherpfennig K, Wiley D (2001). "Structure of a human insulin peptide-HLA-DQ8 complex and susceptibility to type 1 diabetes.". Nat Immunol 2 (6): 501-7. PMID 11376336.
- ^ derived from IMGT/HLA
- ^ a b Layrisse Z, Guedez Y, Domínguez E, Paz N, Montagnani S, Matos M, Herrera F, Ogando V, Balbas O, Rodríguez-Larralde A (2001). "Extended HLA haplotypes in a Carib Amerindian population: the Yucpa of the Perija Range.". Hum Immunol 62 (9): 992-1000. PMID 11543901.
- ^ Gómez-Casado E, Martínez-Laso J, Moscoso J, Zamora J, Martin-Villa M, Perez-Blas M, Lopez-Santalla M, Lucas Gramajo P, Silvera C, Lowy E, Arnaiz-Villena A (2003). "Origin of Mayans according to HLA genes and the uniqueness of Amerindians.". Tissue Antigens 61 (6): 425-36. PMID 12823766.
- ^ Arnaiz-Villena A, Vargas-Alarcón G, Granados J, Gómez-Casado E, Longas J, Gonzales-Hevilla M, Zuñiga J, Salgado N, Hernández-Pacheco G, Guillen J, Martinez-Laso J (2000). "HLA genes in Mexican Mazatecans, the peopling of the Americas and the uniqueness of Amerindians.". Tissue Antigens 56 (5): 405-16. PMID 11144288.
- ^ Moscoso J, Seclen S, Serrano-Vela J, Villena A, Martinez-Laso J, Zamora J, Moreno A, Ira-Cachafeiro J, Arnaiz-Villena A (2006). "HLA genes in Lamas Peruvian-Amazonian Amerindians.". Mol Immunol 43 (11): 1881-9. PMID 16337001.
- ^ Hollenbach J, Thomson G, Cao K, Fernandez-Vina M, Erlich H, Bugawan T, Winkler C, Winter M, Klitz W (2001). "HLA diversity, differentiation, and haplotype evolution in Mesoamerican Natives.". Hum Immunol 62 (4): 378-90. PMID 11295471.
- ^ Leffell M, Fallin M, Hildebrand W, Cavett J, Iglehart B, Zachary A (2004). "HLA alleles and haplotypes among the Lakota Sioux: report of the ASHI minority workshops, part III.". Hum Immunol 65 (1): 78-89. PMID 14700599.
- ^ Lázaro A, Moraes M, Marcos C, Moraes J, Fernández-Viña M, Stastny P (1999). "Evolution of HLA-class I compared to HLA-class II polymorphism in Terena, a South-American Indian tribe.". Hum Immunol 60 (11): 1138-49. PMID 10600013.
- ^ Matsuzaka Y, Makino S, Nakajima K, Tomizawa M, Oka A, Bahram S, Kulski J, Tamiya G, Inoko H (2001). "New polymorphic microsatellite markers in the human MHC class III region.". Tissue Antigens 57 (5): 397-404. PMID 11556964.
- ^ Kuffner T, Whitworth W, Jairam M, McNicholl J (2003). "HLA class II and TNF genes in African Americans from the Southeastern United States: regional differences in allele frequencies.". Hum Immunol 64 (6): 639-47. PMID 12770797.
- ^ a b Nelson J, Boyer G, Templin D, Lanier A, Barrington R, Nisperos B, Smith A, Mickelson E, Hansen J (1992). "HLA antigens in Tlingit Indians with rheumatoid arthritis.". Tissue Antigens 40 (2): 57-63. PMID 1412417.
- ^ Leffell M, Fallin M, Erlich H, Fernandez-Vĩna M, Hildebrand W, Mack S, Zachary A (2002). "HLA antigens, alleles and haplotypes among the Yup'ik Alaska natives: report of the ASHI Minority Workshops, Part II.". Hum Immunol 63 (7): 614-25. PMID 12072196.
- ^ a b Welinder L, Graugaard B, Madsen M (2000). "HLA antigen and gene frequencies in Eskimos of East Greenland.". Eur J Immunogenet 27 (2): 93-7. PMID 10792425.
- ^ a b Lou H, Li H, Kuwayama M, Yashiki S, Fujiyoshi T, Suehara M, Osame M, Yamashita M, Hayami M, Gurtsevich V, Ballas M, Imanishi T, Sonoda S (1998). "HLA class I and class II of the Nivkhi, an indigenous population carrying HTLV-I in Sakhalin, Far Eastern Russia.". Tissue Antigens 52 (5): 444-51. PMID 9864034.
- ^ Sidney J, del Guercio MF, Southwood S, and Sette A. (2002). "The HLA molecules DQA1*0501/B1*0201 and DQA1*0301/B1*0302 share an extensive overlap in peptide binding specificity.". J Immunol. 169 (9): 5098-5108. PMID: 12391226.
- ^ Farjadian S, Moqadam F, Ghaderi A (2006). "HLA class II gene polymorphism in Parsees and Zoroastrians of Iran.". Int J Immunogenet 33 (3): 185-91. PMID 16712649.
- ^ a b Machulla H, Batnasan D, Steinborn F, Uyar F, Saruhan-Direskeneli G, Oguz F, Carin M, Dorak M (2003). "Genetic affinities among Mongol ethnic groups and their relationship to Turks.". Tissue Antigens 61 (4): 292-9. PMID 12753667.
- ^ Liu Y, Liu Z, Fu Y, Jia Z, Chen S, Xu A (2006). "Polymorphism of HLA class II genes in Miao and Yao nationalities of Southwest China.". Tissue Antigens 67 (2): 157-9. PMID 16441488.
- ^ Fu Y, Liu Z, Lin J, Jia Z, Chen W, Pan D, Liu Y, Zhu Y, Chen R, Xu A (2003). "HLA-DRB1, DQB1 and DPB1 polymorphism in the Naxi ethnic group of South-western China.". Tissue Antigens 61 (2): 179-83. PMID 12694588.
- ^ Bannai M, Tokunaga K, Imanishi T, Harihara S, Fujisawa K, Juji T, Omoto K (1996). "HLA class II alleles in Ainu living in Hidaka District, Hokkaidō, northern Japan.". Am J Phys Anthropol 101 (1): 1-9. PMID 8876810.
- ^ Zhou L, Lin B, Xie Y, Liu Z, Yan W, Xu A (2005). "Polymorphism of human leukocyte antigen-DRB1, -DQB1, and -DPB1 genes of Shandong Han population in China.". Tissue Antigens 66 (1): 37-43. PMID 15982255.
- ^ Chimge N, Tanaka H, Kashiwase K, Ayush D, Tokunaga K, Saji H, Akaza T, Batsuuri J, Juji T (1997). "The HLA system in the population of Mongolia.". Tissue Antigens 49 (5): 477-83. PMID 9174140.
- ^ a b Uinuk-Ool T, Takezaki N, Derbeneva O, Volodko N, Sukernik R (2004). "Variation of HLA class II genes in the Nganasan and Ket, two aboriginal Siberian populations.". Eur J Immunogenet 31 (1): 43-51. PMID 15009181.
- ^ Lee K, Oh D, Lee C, Yang S (2005). "Allelic and haplotypic diversity of HLA-A, -B, -C, -DRB1, and -DQB1 genes in the Korean population.". Tissue Antigens 65 (5): 437-47. PMID 15853898.
- ^ Saito S, Ota S, Yamada E, Inoko H, Ota M (2000). "Allele frequencies and haplotypic associations defined by allelic DNA typing at HLA class I and class II loci in the Japanese population.". Tissue Antigens 56 (6): 522-9. PMID 11169242.
- ^ Mizuki N, Ohno S, Ando H, Sato T, Imanishi T, Gojobori T, Ishihara M, Goto K, Ota M, Geng Z, Geng L, Li G, Inoko H (1998). "Major histocompatibility complex class II alleles in an Uygur population in the Silk Route of Northwest China.". Tissue Antigens 51 (3): 287-92. PMID 9550330.
- ^ Mizuki M, Ohno S, Ando H, Sato T, Imanishi T, Gojobori T, Ishihara M, Ota M, Geng Z, Geng L, Li G, Kimura M, Inoko H (1997). "Major histocompatibility complex class II alleles in Kazak and Han populations in the Silk Route of northwestern China.". Tissue Antigens 50 (5): 527-34. PMID 9389328.
- ^ Uinuk-Ool T, Takezaki N, Sukernik R, Nagl S, Klein J (2002). "Origin and affinities of indigenous Siberian populations as revealed by HLA class II gene frequencies.". Hum Genet 110 (3): 209-26. PMID 11935333.
- ^ Velickovic Z, Delahunt B, Carter J (2002). "HLA-DRB1 and HLA-DQB1 polymorphisms in Pacific Islands populations.". Tissue Antigens 59 (5): 397-406. PMID 12144623.
- ^ a b c d Evseeva I, Spurkland A, Thorsby E, Smerdel A, Tranebjaerg L, Boldyreva M, Groudakova E, Gouskova I, Alexeev L (2002). "HLA profile of three ethnic groups living in the North-Western region of Russia.". Tissue Antigens 59 (1): 38-43. PMID 11972877.
- ^ Arnaiz-Villena A, Elaiwa N, Silvera C, Rostom A, Moscoso J, Gómez-Casado E, Allende L, Varela P, Martínez-Laso J (2001). "The origin of Palestinians and their genetic relatedness with other Mediterranean populations.". Hum Immunol 62 (9): 889-900. PMID 11543891.
- ^ a b c d e f g h i Kimiyoshi, Tsuji; Aizawa M and Sasazuki T (1992 location = Oxford). Proceedings of the Eleventh International Histocompatibility Workshop and Conference Held in Yokohoma, Japan, 6-13 November, 1991. Oxford University Press. ISBN 0-19-262390-7.
- ^ Doherty D, Vaughan R, Donaldson P, Mowat A (1992). "HLA DQA, DQB, and DRB genotyping by oligonucleotide analysis: distribution of alleles and haplotypes in British caucasoids.". Hum Immunol 34 (1): 53-63. PMID 1399722.
- ^ "12th International Histocompatibility Conference. Genetic diversity of HLA: functional and medical implications. Paris, France, June 9-12, 1996. Abstracts.". Hum Immunol 47 (1-2): 1-184. PMID 8909580.
- ^ Bugawan T, Klitz W, Blair A, Erlich H (2000). "High-resolution HLA class I typing in the CEPH families: analysis of linkage disequilibrium among HLA loci.". Tissue Antigens 56 (5): 392-404. PMID 11144287.
- ^ Schipper R, Schreuder G, D'Amaro J, Oudshoorn M (1996). "HLA gene and haplotype frequencies in Dutch blood donors.". Tissue Antigens 48 (5): 562-74. PMID 8988539.
- ^ Kapustin S, Lyshchov A, Alexandrova J, Imyanitov E, Blinov M (1999). "HLA class II molecular polymorphisms in healthy Slavic individuals from North-Western Russia.". Tissue Antigens 54 (5): 517-20. PMID 10599891.
- ^ Sanchez-Velasco P, Gomez-Casado E, Martinez-Laso J, Moscoso J, Zamora J, Lowy E, Silvera C, Cemborain A, Leyva-Cobián F, Arnaiz-Villena A (2003). "HLA alleles in isolated populations from North Spain: origin of the Basques and the ancient Iberians.". Tissue Antigens 61 (5): 384-92. PMID 12753657.
- ^ Valluri V, Valluei V, Mustafa M, Santhosh A, Middleton D, Alvares M, Alvales M, El Haj E, Gumama O, Abdel-Wareth L, Abdel-Waieth L (2005). "Frequencies of HLA-A, HLA-B, HLA-DR, and HLA-DQ phenotypes in the United Arab Emirates population.". Tissue Antigens 66 (2): 107-13. PMID 16029430.
- ^ Sánchez-Velasco P, Karadsheh N, García-Martín A, Ruíz de Alegría C, Leyva-Cobián F (2001). "Molecular analysis of HLA allelic frequencies and haplotypes in Jordanians and comparison with other related populations.". Hum Immunol 62 (9): 901-9. PMID 11543892.
- ^ a b Fort M, de Stefano G, Cambon-Thomsen A, Giraldo-Alvarez P, Dugoujon J, Ohayon E, Scano G, Abbal M (1998). "HLA class II allele and haplotype frequencies in Ethiopian Amhara and Oromo populations.". Tissue Antigens 51 (4 Pt 1): 327-36. PMID 9583804.
- ^ Gómez-Casado E, del Moral P, Martínez-Laso J, García-Gómez A, Allende L, Silvera-Redondo C, Longas J, González-Hevilla M, Kandil M, Zamora J, Arnaiz-Villena A (2000). "HLA genes in Arabic-speaking Moroccans: close relatedness to Berbers and Iberians.". Tissue Antigens 55 (3): 239-49. PMID 10777099.
- ^ Ayed K, Ayed-Jendoubi S, Sfar I, Labonne M, Gebuhrer L (2004). "HLA class-I and HLA class-II phenotypic, gene and haplotypic frequencies in Tunisians by using molecular typing data.". Tissue Antigens 64 (4): 520-32. PMID 15361135.
- ^ a b Renquin J, Sanchez-Mazas A, Halle L, Rivalland S, Jaeger G, Mbayo K, Bianchi F, Kaplan C (2001). "HLA class II polymorphism in Aka Pygmies and Bantu Congolese and a reassessment of HLA-DRB1 African diversity.". Tissue Antigens 58 (4): 211-22. PMID 11782272.
- ^ Pimtanothai N, Hurley C, Leke R, Klitz W, Johnson A (2001). "HLA-DR and -DQ polymorphism in Cameroon.". Tissue Antigens 58 (1): 1-8. PMID 11580849.
- ^ Schnittger L, May J, Loeliger C, Gallin M, Erttmann K, Bienzle U, Kremsner P, Meyer C (1997). "HLA DRB1-DQA1-DQB1 haplotype diversity in two African populations.". Tissue Antigens 50 (5): 546-51. PMID 9389330.
- ^ de Pablo R, García-Pacheco J, Vilches C, Moreno M, Sanz L, Rementería M, Puente S, Kreisler M (1997). "HLA class I and class II allele distribution in the Bubi population from the island of Bioko (Equatorial Guinea).". Tissue Antigens 50 (6): 593-601. PMID 9458112.
- ^ Park Y, Tait B, Kawasaki E, Rowley M, Mackay I. "Closer association of IA-2 humoral autoreactivity with HLA DR3/4 than DQB1*0201/*0302 in Korean T1D patients.". Ann N Y Acad Sci 1037: 104-9. PMID 15699500.
- ^ Hermann R, Turpeinen H, Laine A, Veijola R, Knip M, Simell O, Sipilä I, Akerblom H, Ilonen J (2003). "HLA DR-DQ-encoded genetic determinants of childhood-onset type 1 diabetes in Finland: an analysis of 622 nuclear families.". Tissue Antigens 62 (2): 162-9. PMID 12889996.
Links
Coeliac Disease
- Coeliac UK (charity)
- The Celiac Disease Foundation (U.S.)
- The Celiac Sprue Association (U.S.)
- National Digestive Diseases Clearinghouse - page on coeliac disease
- National Foundation for Celiac Awareness (U.S.)
- University of Maryland Center for Celiac Research
Type 1 Diabetes
|