To use all functions of this page, please activate cookies in your browser.
my.chemeurope.com
With an accout for my.chemeurope.com you can always see everything at a glance – and you can configure your own website and individual newsletter.
- My watch list
- My saved searches
- My saved topics
- My newsletter
Diabetes mellitus type 1
Diabetes mellitus type 1 (Type 1 diabetes, Type I diabetes, T1D, IDDM) is a form of diabetes mellitus. Type 1 diabetes is an autoimmune disease that results in the permanent destruction of insulin producing beta cells of the pancreas. Type 1 is lethal unless treatment with exogenous insulin via injections replaces the missing hormone. Type 1 diabetes (formerly known as "childhood", "juvenile" or "insulin-dependent" diabetes) is not exclusively a childhood problem: the adult incidence of Type 1 is significant — many adults who contract Type 1 diabetes are misdiagnosed with Type 2 due to the misconception of Type 1 as a disease of children — and since there is no cure, Type 1 diabetic children will grow up to be Type 1 diabetic adults. There is currently no preventive measure that can be taken against type 1 diabetes. Most people affected by type 1 diabetes are otherwise healthy and of a healthy weight when onset occurs, but they can lose weight quickly and dangerously, if not diagnosed in a relatively short amount of time. Diet and exercise cannot reverse or prevent type 1 diabetes. However, there are clinical trials ongoing that aim to find methods of preventing or slowing its development. The most useful laboratory test to distinguish Type 1 from Type 2 diabetes is the C-peptide assay, which is a measure of endogenous insulin production since external insulin (to date) has included no C-peptide. However, C-peptide is not absent in Type 1 diabetes until insulin production has fully ceased, which may take months[citation needed]. The presence of anti-islet antibodies (to Glutamic Acid Decarboxylase, Insulinoma Associated Peptide-2 or insulin), or lack of insulin resistance, determined by a glucose tolerance test, would also be suggestive of Type 1. As opposed to that, many Type 2 diabetics still produce some insulin internally, and all have some degree of insulin resistance. Testing for GAD 65 antibodies has been proposed as an improved test for differentiating between Type 1 and Type 2 diabetes.
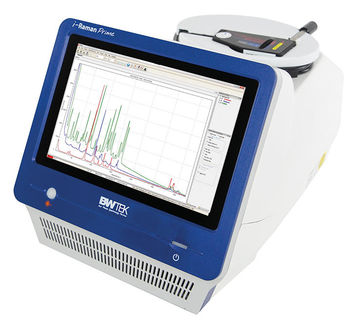
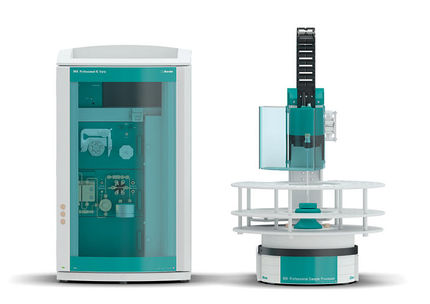
Product highlight
PathophysiologyThe cause of Type 1 diabetes is still not understood. Type 1 diabetes could be a virally induced autoimmune response. Autoimmunity is a condition where one's own immune system "attacks" structures in one's own body either destroying the tissue or decreasing its functionality. In the proposed scenario, pancreatic beta cells in the Islets of Langerhans are destroyed or damaged sufficiently to abolish endogenous insulin production. This etiology makes type 1 distinct from type 2 diabetes mellitus. It should also be noted that the use of insulin in a patient's diabetes treatment protocol does not render them as having type 1 diabetes, the type of diabetes a patient has is determined only by disease etiology. The autoimmune attack may be triggered by reaction to an infection, for example by one of the viruses of the Coxsackie virus family or German measles, although the evidence is inconclusive. This vulnerability is not shared by everyone, for not everyone infected by these organisms develops Type 1 diabetes. This has suggested a genetic vulnerability and there is indeed an observed inherited tendency to develop Type 1[citation needed]. It has been traced to particular HLA phenotypes, though the connection between them and the triggering of an auto-immune reaction is poorly understood. Some researchers believe that the autoimmune response is influenced by antibodies against cow's milk proteins. A large retrospective controlled study published in 2006 strongly suggests that infants who were never breast fed had twice the risk for developing Type 1 diabetes as infants who were breast fed for at least three months. The mechanism, if any, is not understood. No connection has been established between autoantibodies, antibodies to cow's milk proteins, and Type 1 diabetes. A subtype of Type 1 (identifiable by the presence of antibodies against beta cells) typically develops slowly and so is often confused with Type 2. In addition, a small proportion of Type 1 cases have the hereditary condition maturity onset diabetes of the young (MODY) which can also be confused with Type 2. Vitamin D in doses of 2000 IU per day given during the first year of a child's life has been connected in one study in Northern Finland (where intrinsic production of Vitamin D is low due to low natural light levels) with a reduction in the risk of getting Type 1 diabetes later in life (by 80%). Some suggest that Vitamin D3 (one of several related chemicals with Vitamin D activity) may be an important pathogenic factor in Type 1 diabetes independent of geographical latitude. Some chemicals and drugs specifically destroy pancreatic cells. Vacor (N-3-pyridylmethyl-N'-p-nitrophenyl urea), a rodenticide introduced in the United States in 1976, selectively destroys pancreatic beta cells, resulting in Type 1 diabetes after accidental or intentional ingestion. Vacor was withdrawn from the U.S. market in 1979. Zanosar is the trade name for streptozotocin, an antibiotic and antineoplastic agent used in chemotherapy for pancreatic cancer, that kills beta cells, resulting in loss of insulin production. Other pancreatic problems, including trauma, pancreatitis or tumors (either malignant or benign), can also lead to loss of insulin production. The exact cause(s) of Type 1 diabetes are not yet fully understood, and research on those mentioned, and others, continues. TreatmentType 1 is treated with insulin replacement therapy — usually by injection or insulin pump, dietary control, typically including carbohydrate tracking, and careful monitoring of blood glucose levels using Glucose meters. Untreated Type 1 diabetes can lead to one form of diabetic coma, diabetic ketoacidosis, which can be fatal. At present, insulin treatment must be continued for a lifetime; this will change if better treatment, or a cure, is discovered. Continuous glucose monitors have been developed which alert to the presence of dangerously high or low blood sugar levels. In some extreme cases, a pancreas transplant can help restore proper glucose regulation. However, the surgery and accompanying immunosuppression required is considered by many physicians to be more dangerous than continued insulin replacement therapy and is therefore often used only as a last resort (such as when a kidney must also be transplanted or in cases where the patient's blood glucose levels are extremely control resistant). Experimental replacement of beta cells (by transplant or from stem cells) is being investigated in several research programs and may become clinically available in the future. Thus far, beta cell replacement has only been performed on patients over age 18, and with tantalizing successes amidst with nearly universal failure. Pancreas transplantationPancreas transplants are not generally recommended because introducing a new, functioning pancreas to a patient with diabetes can have negative effects on the patient's normally functioning kidney. Artificial PancreasPrevalenceIt is estimated that about 5%–10% of North American diabetes patients have type 1. The fraction of type 1 in other parts of the world differs; this is likely due to both differences in the rate of type 1 and differences in the rate of other types, most prominently type 2. Most of this difference is not currently understood. Variable criteria for categorizing diabetes types may play a part. Research foundationsThe major charitable organization in the USA devoted to type 1 diabetes research is the Juvenile Diabetes Research Foundation (JDRF), whose mission is to cure type 1 diabetes and its complications through the support of research. Since its founding in 1970, JDRF has contributed more than $1 billion to diabetes research, including more than $137 million in FY 2007. In FY2007, the Foundation funded 700 centers, grants and fellowships in 20 countries. The International Diabetes Federation is a worldwide alliance of over 160 countries to address diabetes research and treatment. The American Diabetes Association funds some work on type 1 but devotes much of its resources to type 2 diabetes due to the increasing prevalence of the latter type. Diabetes Australia is involved in promoting research and education in Australia on both type 1 and type 2 diabetes. CureAs of 2007, there is no known cure for diabetes mellitus type 1.[1] There is ongoing research on various approaches to curing diabetes type 1. Diabetes type 1 is caused by the non-existence of a sufficient number of beta cells in the body; these cells, which are found in the Langerhans islets in the pancreas, produce and secrete insulin, the single hormone responsible for allowing glucose to enter from the blood into cells. Hence, the phrase "curing diabetes type 1" means "causing a maintenance or restoration of the endogenous ability of the body to produce insulin in response to the level of blood glucose". This section does not deal with approaches other than that (for instance, closed-loop integrated glucometer/insulin pump products), which may also greatly increase quality of life for those who have diabetes type 1, and may by some be termed "artificial pancreas". Instead, it only deals with such approaches for thoroughly curing the underlying condition of diabetes type 1, by enabling the body to endogenously, in vivo, produce insulin in response to the level of blood glucose. ReversionEncapsulation approach
A biological approach to the artificial pancreas is to implant bioengineered tissue containing islet cells, which would secrete the amounts of insulin, amylin and glucagon needed in response to sensed glucose. When islet cells have been transplanted via the Edmonton protocol, insulin production (and glycemic control) was restored, but at the expense of immunosuppression. Encapsulation of the islet cells in a protective coating has been developed to block the immune response to transplanted cells, which relieves the burden of immunosuppression and benefits the longevity of the transplant.[2] One concept of the bio-artificial pancreas uses encapsulated islet cells to build an islet sheet which can be surgically implanted to function as an artificial pancreas.[3] This islet sheet design consists of:
Islet sheet with encapsulation research is pressing forward with large animal studies at the present, with plans for human clinical trials within a few years. Islet cell transplantation approachLess invasive than a pancreas transplant, islet cell transplantation is considered a very promising approach to curing type 1 diabetes. In one variant of this procedure, islet cells are injected into the patient's liver, where they take up residence and begin to produce insulin. The liver is expected to be the most reasonable choice because it is more accessible than the pancreas, and the islet cells seem to produce insulin well in that environment. The patient's body, however, will treat the new cells just as it would any other introduction of foreign tissue. The immune system will attack the cells as it would a bacterial infection or a skin graft. Thus, the patient also needs to undergo treatment involving immunosuppressants, which reduce immune system activity. Recent studies have shown that islet cell transplants have progressed to the point that 58% of the patients in one study were insulin independent one year after the operation.[4] It would be best to use islet cells which will not provoke this immune reaction. Islet cell regeneration approachResearch undertaken at the Massachusetts General Hospital in Boston Masschusetts from 2001 and 2003 demonstrated a protocol to reverse type 1 diabetes in mice.[5] Three other institutions have had similar results, published in the March 24, 2006 issue of Science. A fourth study by the National Institutes of Health further confirmed the approach, and also sheds light on the biological mechanisms involved.[6] Stem cells approachResearch is being done at several locations in which islet cells are developed from stem cells. In January 2006, a team of South Korean scientists has grown pancreatic beta cells, which can help treat diabetes, from stem cells taken from the umbilical cord blood of newborn babies. In April 2007, it was reported by the Times Online that 15 young Brazilian patients diagnosed with Type 1 diabetes were able to naturally produce insulin once again after undergoing mild chemotherapy to temporarily weaken their immune systems and then injection of their own stem cells. This allowed the pancreatic beta cells to produce insulin. Since white blood cells were blocking the pancreas from producing insulin, Dr. Voltarelli and colleagues killed the immune cells, allowing the pancreas to secrete insulin once more. However, there were no control subjects, which means that all of the processes could have been completely or partially natural. Secondly, no theory for the mechanism of cure has been promoted. It is too early to say whether the results will be positive or negative in the long run.[7] Gene therapy approachTechnology for gene therapy is advancing rapidly such that there are multiple pathways possible to support endocrine function, with potential to practically cure diabetes.[8]
Yonsei University studyScientists in the South Korean university of Yonsei have, in 2000, succeeded in reversing diabetes in mice and rats. Using a viral vector, a DNA encoding the production of an insulin analog was injected to the animals, which remained non-diabetic for at least the eight months duration of the study.[12] Nanotechnology approachUnder the nanotechnological approach to curing diabetes type 1, many "nanobots" would be injected into the patient's bloodstream. These nanobots would be able to synthesize insulin, and to secrete it according to the level of glucose they would sense.[13] Nano MistAn American body called "Nano Mist" claims to be involved in a diabetes cure-related nanotechnology project. Their product is at least 10 years behind FDA approval.[14] Prevention"Immunization" approachIf a biochemical mechanism can be found that prevents the immune system from attacking beta cells, it may be administered to prevent commencement of diabetes type 1. The way several groups are trying to achieve this is by causing the activation state of the immune system to change from Th1 state (“attack” by killer T Cells) to Th2 state (development of new antibodies). This Th1-Th2 shift occurs via a change in the type of cytokine signaling molecules being released by regulatory T-cells. Instead of pro-inflammatory cytokines, the regulatory T-cells begin to release cytokines that inhibit inflammation.[1] This phenomenon is commonly known as "acquired immune tolerance". DiaPep277A substance designed to cause lymphocyte cells to cease attacking beta cells, DiaPep277 is a peptide fragment of a larger protein called HSP60. Given as a subcutaneous injection, its mechanism of action involves a Th1-Th2 shift. Clinical success has been demonstrated in prolonging the "honeymoon" period for people who already have type 1 diabetes [2]. The product is currently being tested in people with latent autoimmune diabetes of adults (LADA). Intra-nasal insulinThere is pre-clinical evidence that a Th1-Th2 shift can be induced by administration of insulin directly onto the immune tissue in the nasal cavity. This observation has led to a clinical trial, called INIT II, which began in late 2006, based in Australia and New Zealand. Denise Faustman researchRelationship with nervous and immune systems approachIn December 2006, researchers from Toronto Hospital for Sick Children revealed research that shows a link between type 1 diabetes and the immune and nervous system. Using mice, the researchers discovered that a control circuit exists between insulin-producing cells and their associated sensory (pain-related) nerves.[15] It's being suggested that faulty nerves in the pancreas could be a cause of type 1 diabetes. Entities involved in researchThis section is a complete list of mainly commercial companies but also other entities, namely governmental institutions and individual persons, actively involved in research towards finding a cure to diabetes type 1. Entities are listed along with their status of research in that field, so that also entities which ceased research into finding a cure to diabetes type 1 may be listed. Entities are alphabetically listed.
Further reading
References
|
||||||||||||||||||||||||||||||||||||||||
| This article is licensed under the GNU Free Documentation License. It uses material from the Wikipedia article "Diabetes_mellitus_type_1". A list of authors is available in Wikipedia. | ||||||||||||||||||||||||||||||||||||||||