To use all functions of this page, please activate cookies in your browser.
my.chemeurope.com
With an accout for my.chemeurope.com you can always see everything at a glance – and you can configure your own website and individual newsletter.
- My watch list
- My saved searches
- My saved topics
- My newsletter
Amiodarone
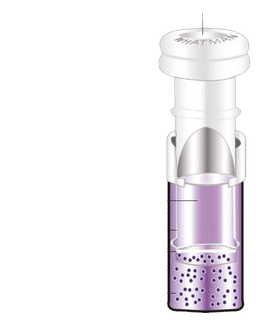
Amiodarone is an antiarrhythmic agent (medication used for irregular heart beat) used for various types of tachyarrhythmias (fast forms of irregular heart beat), both ventricular and supraventricular (atrial) arrhythmias. Discovered in 1961, it was not approved for use in the United States until 1985. Despite relatively common side-effects, it is used in arrhythmias that are otherwise difficult to treat with medication. Related newer compounds, such as dronedarone, may have similar efficacy but a reduced rate of side-effects. Product highlight
HistoryAmiodarone was initially developed in 1961 at the Labaz company, Belgium, by chemists Tondeur and Binon. It became popular in Europe as a treatment for angina pectoris.[1][2] As a doctoral candidate at Oxford University, Dr. Bramah Singh determined that amiodarone and sotalol had antiarrhythmic properties and belonged to a new class of antiarrhythmic agents (what would become the class III antiarrhythmic agents).[3] Today the mechanisms of action of amiodarone and sotalol remain unknown. It is thought to involve prolonging the action potential duration, prolonging the refractory period, or interacting with K+ channels. Based on Singh's work, the Argentinian physician Dr. Mauricio Rosenbaum began using amiodarone to treat his patients who suffered from supraventricular and ventricular arrhythmias, with impressive results. Based on papers written by Dr. Rosenbaum developing Singh's theories, physicians in the United States began prescribing amiodarone to their patients with potentially life-threatening arrhythmias in the late 1970s.[4][5] By 1980, amiodarone was commonly prescribed throughout Europe for the treatment of arrhythmias, but in the U.S. amiodarone remained unapproved by the Food and Drug Administration, and physicians were forced to directly obtain amiodarone from pharmaceutical companies in Canada and Europe.[citation needed] The FDA was reluctant to officially approve the use of amiodarone, since initial reports had shown increased incidence of serious pulmonary side-effects of the drug. In the mid 1980s, the European pharmaceutical companies began putting pressure on the FDA to approve amiodarone by threatening to cut the supply to American physicians if it were not approved. In December of 1985, amiodarone was approved by the FDA for the treatment of arrhythmias.[6] This makes amiodarone one of the few drugs approved by the FDA without rigorous randomized clinical trials. DosingAmiodarone is available in oral and intravenous formulations. Orally, it is available under the trade names Pacerone® (produced by Upsher-Smith Laboratories, Inc.) and Cordarone® (produced by Wyeth-Ayerst Laboratories) in 200mg and 400 mg tablets; It is also available under the trade name Aratac® (produced by Alphapharm Pty Ltd) in 100 mg and 200 mg tablets in Australia and New Zealand. Also Arycor® in South Africa (Produced by Winthrop Pharmaceuticals.) in doses of 100mg and 200mg scored tablets. In South America, it is known as Atlansil® and is produced by Roemmers. It is also available in intravenous ampules and vials, typically in 150 mg increments. The dose of amiodarone administered is tailored to the individual and the dysrhythmia that is being treated. When administered orally, the bioavailability of amiodarone is quite variable. Absorption ranges from 22 to 95%, with better absorption when it is given with food.[7] Amiodarone is fat-soluble, and tends to concentrate in tissues including fat, muscle, liver, lungs, and skin. This confers a high volume of distribution (5000 liters in a 70 kg adult) and a long half-life. Due to the long half-life of amiodarone, oral loading typically takes days to weeks. An oral loading dose is typically a total of 10 grams, divided over one to two weeks but there are many other dosing regimens. Once an individual is loaded, a typical maintenance dose of amiodarone is 100 or 200 mg either once or twice daily. An intravenous loading dose is typically 300 mg in 20-30cc D5W for cardiac arrest. The loading infusion for dysrhythmias is typically 150 mg in a 100cc bag of D5W given over 10 minutes. Both can be followed by a 360 mg slow infusion over 6 hours then a maintenance infusion of 540 mg over 18 hours. Mechanism of actionAmiodarone is categorized as a class III antiarrhythmic agent, and prolongs phase 3 of the cardiac action potential. It has numerous other effects however, including actions that are similar to those of antiarrhythmic classes Ia, II, and IV. Amiodarone shows beta blocker-like and calcium channel blocker-like actions on the SA and AV nodes, increases the refractory period via sodium- and potassium-channel effects, and slows intra-cardiac conduction of the cardiac action potential, via sodium-channel effects. Indications for useBecause amiodarone has a low incidence of pro-arrhythmic effects, it has been used both in the treatment of acute life-threatening arrhythmias as well as the chronic suppression of arrhythmias. It is useful both in supraventricular arrhythmias and ventricular arrhythmias. Ventricular fibrillationThe treatment of choice for ventricular fibrillation (VF) is electrical defibrillation. However, amiodarone can be useful in shock-refractory VF. In the ARREST trial, amiodarone was shown to improve survival to hospital admission (when compared to placebo) in individuals who suffer cardiac arrest with shock-refractory VF.[8] It is on the basis of this study that the guidelines created by the American Heart Association for the treatment of VF include amiodarone as a second line agent (after epinephrine or vasopressin). ARREST was not adequately powered to demonstrate survival to hospital discharge. Ventricular tachycardiaAmiodarone may be used in the treatment of ventricular tachycardia in certain instances. Individuals with hemodynamically unstable ventricular tachycardia should not initially receive amiodarone. These individuals should be cardioverted out of their unstable rhythm. Amiodarone can be used in individuals with hemodynamically stable ventricular tachycardia. In these cases, amiodarone can be used regardless of the individual's underlying heart function and the type of ventricular tachycardia; it can be used in individuals with monomorphic ventricular tachycardia as well as individuals with polymorphic ventricular tachycardia. The dose of amiodarone is 150 mg IV administered over 10 minutes. Atrial fibrillationIndividuals who have undergone open heart surgery are at an increased risk of developing atrial fibrillation (or AF) in the first few days post-procedure. In the ARCH trial, intravenous amiodarone (2 grams administered over 2 days) has been shown to reduce the incidence of atrial fibrillation after open heart surgery when compared to placebo.[9] However, clinical studies have failed to demonstrate long-term efficacy and have shown potentially fatal side effects such as pulmonary toxicities. While Amiodarone is not approved for AF by the FDA, it is a commonly prescribed off-label treatment due to the lack of efficacious treatment alternatives. So called 'acute onset atrial fibrillation', defined by the North American Society of Pacing and Electrophysiology (NASPE)in 2003, responds well to short duration treatment with amiodarone. This has been demonstrated in seventeen randomised controlled trials, of which five included a placebo arm. The incidence of severe side effects in this group is low. The benefit of amiodarone in the treatment of atrial fibrillation in the critical care population has yet to be determined but it may prove to be the agent of choice where the patient is haemodynamically unstable and unsuitable for DC cardioversion. It is recommended in such a role by the UK government's National Institute for Health and Clinical Excellence (NICE). ContraindicationsThe only absolute contraindications to the administration of amiodarone is allergic reaction (ie: anaphylaxis) to the compound. However, because of the wide spectrum of the mechanism of action of amiodarone and the numerous side effects possible, there are a number of groups for which care should be taken when administering the drug. Individuals who are pregnant or may become pregnant are strongly advised to not take amiodarone. Since amiodarone can be expressed in breast milk, women taking amiodarone are advised to stop nursing. It is contraindicated in individuals with sinus nodal bradycardia, atrioventricular block, and second or third degree heart block who do not have an artificial pacemaker. Individuals with baseline depressed lung function should be monitored closely if amiodarone therapy is to be initiated. The injection should not be given to neonates, because the benzyl alcohol it contains may cause the fatal "gasping syndrome". Amiodarone can worsen the cardiac arrhythmia brought on by Foxglove poisoning. MetabolismAmiodarone is extensively metabolized in the liver, and can affect the metabolism of numerous other drugs. The major metabolite of amiodarone is desethylamiodarone (DEA), which also has antiarrhythmic properties. The metabolism of amiodarone is inhibited by grapefruit juice, leading to elevated serum levels of amiodarone. Interactions with other drugsThe pharmacokinetics of numerous drugs, including many that are commonly administered to individuals with heart disease, are affected by amiodarone. Particularly, doses of digoxin should be halved in individuals taking amiodarone. Amiodarone potentiates the action of warfarin. Individuals taking both of these medications should have their warfarin dose halved and their anticoagulation status (measured as prothrombin time (PT) and international normalized ratio (INR)) measured more frequently. The effect of amiodarone in the warfarin concentration can be as early as a few days after initiation of treatment, or can be delayed a few weeks. Amiodarone inhibits the action of the cytochrome P450 isozyme family. This reduces the clearance of many drugs, including the following: - ExcretionUnlike most other drugs, which are excreted via the urine, excretion is primarily hepatic and biliary with almost no elimination via the renal route and it is not dialyzable [Package Insert- Pacerone(R)]. Elimination half-life average of 58 days (ranging from 25-100 days [Remington: The Science and Practice of Pharmacy 21st edition]) for amiodarone and 36 days for the active metabolite, desethylamiodarone (DEA) [Package Insert- Pacerone(R)]. There is 10-50% transfer of amiodarone and DEA in the placenta as well as presence in breast milk [Package Insert- Pacerone(R)]. Accumulation of amiodarone and DEA occurs in adipose tissue and highly perfused organs (ie. liver, lungs) [Package Insert- Pacerone(R)], therefore, if an individual was taking amiodarone on a chronic basis, if it is stopped it will remain in the system for weeks to months. Side effectsAmiodarone has numerous side effects. Most individuals administered amiodarone on a chronic basis will experience at least one side effect. ThyroidDue to the iodine content of the agent (37.3% by weight), abnormalities in thyroid function are common. Amiodarone is structurally similar to thyroxine (a thyroid hormone), which contributes to the effects of amiodarone on thyroid function. Both under- and overactivity of the thyroid may occur on amiodarone treatment. Measurement of free thyroxine (FT4) alone may be unreliable in detecting these problems and thyroid-stimulating hormone (TSH) should therefore also be checked every 6 months.[10] Hypothyroidism (slowing of the thyroid, called the Wolff-Chaikoff effect) occurs frequently; in the SAFE trial, which compared amiodarone with other medications for the treatment of atrial fibrillation, biochemical hypothyroidism (as defined by a TSH level of 4.5-10 mU/l) occurred in 25.8% of the amiodarone-treated group as opposed to 6.6% of the control group (taking placebo or sotalol). Overt hypothyrodism (defined as TSH >10 mU/l) occurred at 5.0% compared to 0.3%; most of these (>90%) were detected within the first six months of amiodarone treatment.[11] Hyperthyroidism (an overactive thyroid, called the Jodbasedow effect) is less common. In the SAFE trial, the increased rate of hyperthyroidism (5.3% compared to 2.4%) was not statistically significant. Most hyperthyroid patients (defined as TSH <0.35 mU/l) were asymptomatic.[11] Thyroid uptake measurements (I-123 or I-131), which are used to differentiate causes of hyperthyroidism, are generally unreliable in patients who have been taking amiodarone. Because of the high iodine content of amiodarone, the thyroid gland is effectively saturated, thus preventing further uptake of isotopes of iodine. However, the radioactive iodine uptake (nuclear thyroid uptake test) may still be helpful in the diagnosis and management of amiodarone-induced hyperthyroidism.[citation needed] EyeCorneal micro-deposits (Corneal verticillata, also called vortex keratopathy) are almost universally present (over 90%) in individuals taking amiodarone for at least 6 months. These deposits typically do not cause any symptoms. About 1 in 10 individuals may complain of a bluish halo. Optic neuropathy occurs in 1-2% of people and is not dosage dependent. Bilateral optic disk swelling and mild and reversible visual field defects can also occur. Gastrointestinal system and liverAbnormal liver enzyme results are common in patients on amiodarone. Much rarer are jaundice, hepatomegaly (liver enlargement), and hepatitis (inflammation of the liver).[12] Low-dose amiodarone has been reported to cause pseudo-alcoholic cirrhosis.[13][14] SkinLong-term administration of amiodarone is associated with a blue-grey discoloration of the skin, "smurf syndrome." This is more commonly seen in individuals with lighter skin tones. The discoloration may revert upon cessation of the drug. However, the skin color may not return completely to normal. Individuals taking amiodarone may become more sensitive to the harmful effects of UV-A light. Using sunblock that also blocks UV-A rays appears to prevent this side effect. LungThe most serious reaction that is due to amiodarone is interstitial lung disease. The incidence of pulmonary fibrosis is not dose related. Some individuals were noted to develop pulmonary fibrosis after a week of treatment, while others did not develop it after years of continuous use. There are no known factors that increase the incidence of amiodarone-induced pulmonary fibrosis in a particular individual. Common practice is to avoid the agent if possible in individuals with decreased lung function. The most specific test of pulmonary toxicity due to amiodarone is a dramatically decreased DLCO noted on pulmonary function testing. See also
References
Categories: Amines | Antiarrhythmic agents | Aromatic compounds | Ethers | Heterocyclic compounds | Ketones |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| This article is licensed under the GNU Free Documentation License. It uses material from the Wikipedia article "Amiodarone". A list of authors is available in Wikipedia. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||