To use all functions of this page, please activate cookies in your browser.
my.chemeurope.com
With an accout for my.chemeurope.com you can always see everything at a glance – and you can configure your own website and individual newsletter.
- My watch list
- My saved searches
- My saved topics
- My newsletter
Cyclophosphamide
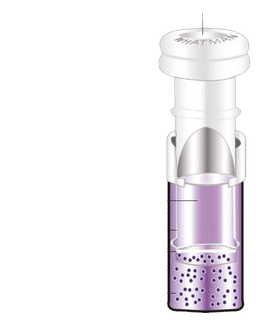
Cyclophosphamide (the generic name for Cytoxan, Neosar), also known as cytophosphane, is a nitrogen mustard alkylating agent, from the oxazophorines group. It is used to treat various types of cancer and some autoimmune disorders. It is a "prodrug"; it is converted in the liver to active forms that have chemotherapeutic activity. Product highlight
UsesThe main use of cyclophosphamide is together with other chemotherapy agents in the treatment of lymphomas, some forms of leukemia and some solid tumors. It is a chemotherapy drug that works by slowing or stopping cell growth. It also works by decreasing the immune system's response to various diseases. In addition, its use is becoming more common in autoimmune diseases where disease-modifying antirheumatic drugs (DMARDs) have been ineffective. Systemic lupus erythematosus (SLE) with severe lupus nephritis, for example, may respond to pulsed cyclophosphamide. However in 2005, standard treatment for lupus nephritis changed to MMF from cyclophosphamide. It is also used to treat Minimal Change Disease and rheumatoid arthritis. It is still used for Wegener's granulomatosis. The trade name is Endoxan. Pharmacokinetics/PharmacodynamicsCyclophosphamide is converted by mixed function oxidase enzymes in the liver to active metabolites. The main active metabolite is 4-hydroxycyclophosphamide. 4-hydroxycyclophosphamide exists in equilibrium with its tautomer, aldophosphamide. Most of the aldophosphamide is oxidised by the enzyme aldehyde dehydrogenase (ALDH) to make carboxyphosphamide. A small proportion of aldophosphamide is converted into phosphoramide mustard and acrolein. Acrolein is toxic to the bladder epithelium and can lead to hemorrhagic cystitis. This can be prevented through the use of aggressive hydration and/or Mesna. Recent clinical studies have shown that cyclophosphamide induce beneficial immunomodulatory effects in the context of adoptive immunotherapy. Although the mechanisms underlying these effects are not fully understood, several mechanisms have been suggested based on potential modulation of the host environment, including[citation needed]:
Thus, cyclophosphamide pre-conditioning of recipient hosts (for donor T cells) has been used to enhance immunity in naïve hosts, and to enhance adoptive T cell immunotherapy regimens as well as active vaccination strategies, inducing objective anti-tumor immunity. Mode of actionThe main effect of cyclophosphamide is due to its metabolite phosphoramide mustard. This metabolite is only formed in cells which have low levels of ALDH. Phosphoramide mustard forms DNA crosslinks between (interstrand crosslinkages) and within (intrastrand crosslinkages) DNA strands at guanine N-7 positions. This leads to cell death. Cyclophosphamide has relatively little typical chemotherapy toxicity as ALDHs are present in relatively large concentrations in bone marrow stem cells, liver and intestinal epithelium. ALDHs protect these actively proliferating tissues against toxic effects phosphoramide mustard and acrolein by converting aldophosphamide to carboxyphosphamide that does not give rise to the toxic metabolites (phosphoramide mustard and acrolein). Side-effectsMany people taking cyclophosphamide do not have serious side effects. Side-effects include chemotherapy-induced nausea and vomiting (CINV), bone marrow suppression, stomach ache, diarrhea, darkening of the skin/nails, alopecia (hair loss) and lethargy. Hemorrhagic cystitis is a frequent complication, but this is prevented by adequate fluid intake and Mesna (sodium 2-mercaptoethane sulfonate). Mesna is a sulfhydryl donor and binds acrolein. Cyclophosphamide is itself carcinogenic, potentially causing transitional cell carcinoma of the bladder as a long-term complication. It can lower the body's ability to fight an infection. It can cause temporary or (rarely) permanent sterility. Although it is used to treat cancer, it may increase the risk of developing another form of cancer, sometimes months to years after treatment. Other (serious) side effects include:
HistoryCyclophosphamide and the related nitrogen mustard-derived alkylating agent ifosfamide were developed by Norbert Brock and ASTA (now Baxter Oncology). Brock and his team synthesised and screened more than 1,000 candidate oxazaphosphorine compounds.[1] They converted the base nitrogen mustard into a non-toxic "transport form". This transport form was a pro-drug, subsequently actively transported into the cancer cells. Once in the cells, the pro-drug was enzymatically converted into the active, toxic form. The first clinical trials were published at the end of the 1950s.[2][3][4] References
Categories: Chemotherapeutic agents | Organochlorides | Phosphorus compounds | Prodrugs | IARC Group 1 carcinogens |
|||||||||||||||||||||||||||||||||||||||||||||||||||||
| This article is licensed under the GNU Free Documentation License. It uses material from the Wikipedia article "Cyclophosphamide". A list of authors is available in Wikipedia. | |||||||||||||||||||||||||||||||||||||||||||||||||||||