To use all functions of this page, please activate cookies in your browser.
my.chemeurope.com
With an accout for my.chemeurope.com you can always see everything at a glance – and you can configure your own website and individual newsletter.
- My watch list
- My saved searches
- My saved topics
- My newsletter
Phenobarbital
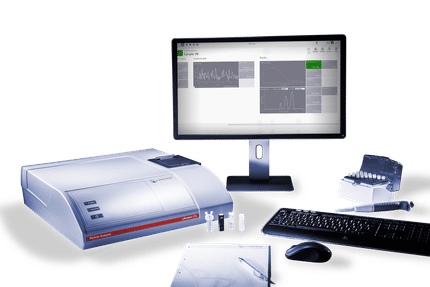
Phenobarbital (INN) or phenobarbitone (former BAN) is a barbiturate, first marketed as Luminal by Farbwerke Fr. Bayer and Co. It is the most widely used anticonvulsant worldwide and the oldest still in use. It also has sedative and hypnotic properties but, as with other barbiturates, has been superseded by the benzodiazepines for these indications. The World Health Organization recommends its use as first-line for partial and generalized tonic-clonic seizures (those formerly known as Grand Mal) in developing countries. It is a core medicine in the WHO Model List of Essential Medicines, which is a list of minimum medical needs for a basic health care system.[1] In more affluent countries, it is no longer recommended as a first or second-line choice anticonvulsant for most seizure types,[2][3] though it is still commonly used to treat neonatal seizures.[4] Product highlight
HistoryThe first barbiturate drug, barbital, was synthesized in 1902 by German chemists Emil Fischer and Joseph von Mering at Bayer. By 1904 several related drugs, including phenobarbital, had been synthesized by Fischer. Phenobarbital was brought to market in 1912 by the drug company Bayer using the brand Luminal. It remained a commonly prescribed sedative and hypnotic until the introduction of benzodiazepines in the 1950s.[5] Phenobarbital's soporific, sedative and hypnotic properties were well known in 1912, but nobody knew it was also an effective anticonvulsant. The young doctor Alfred Hauptmann gave it to his epilepsy patients as a tranquiliser and discovered that their epileptic attacks were susceptible to the drug. Hauptmann performed a careful study of his patients over an extended period. Most of these patients were using the only effective drug then available, bromide, which had terrible side effects and limited efficacy. On phenobarbital, their epilepsy was much improved: the worse patients suffered fewer and lighter seizures and some patients became seizure free. In addition, they improved physically and mentally as bromides were removed from their regime. Patients who had been institutionalised due to the severity of their epilepsy were able to leave and, in some cases, resume employment. Hauptman dismissed concerns that its effectiveness in stalling epileptic attacks could lead to patients suffering a build-up that needed to be "discharged". As he expected, withdrawal of the drug lead to an increase in seizure frequency – it was not a cure. The drug was quickly adopted as the first widely effective anticonvulsant, though World War I delayed its introduction in the U.S.[6] Phenobarbital was used to treat neonatal jaundice by increasing liver metabolism and thus lowering bilirubin levels. In the 1950s, phototherapy was discovered, and became the standard treatment.[7] In 1940, Winthrop Chemical produced sulfathiazole tablets that were contaminated with phenobarbital. This occurred because both tablets were produced side-by-side and equipment could be interchanged. Each antibacterial tablet contained more than twice the required dose of phenobarbital necessary to induce sleep. Hundreds of patients died or were injured as a result. A U.S. Food and Drug Administration investigation was highly critical of Winthrop and the scandal lead to the introduction of Good Manufacturing Practice for drugs.[7] The drug itself through predated FDA approval processes and has failed to be formally cleared for use in subsequent years. Guidance was issued in June 2006 of plans to enforce US approval for unapproved drugs.[8] Phenobarbital was used for over 25 years as prophylaxis in the treatment of febrile seizures.[9] Although an effective treatment in preventing recurrent febrile seizures, it had no positive effect on patient outcome or risk of developing epilepsy. The treatment of simple febrile seizures with anticonvulsant prophylaxis is no longer recommended.[10][11] IndicationsPhenobarbital is indicated in the treatment of all types of seizures except absence seizures.[2][12] Phenobarbital is no less effective at seizure control than more modern drugs such as phenytoin and carbamazepine. It is, however, significantly less well tolerated.[13][14] The first line drugs for treatment of status epilepticus are fast acting benzodiazepines such as diazepam or lorazepam. If these fail then phenytoin may be used, with phenobarbital being an alternative in the U.S. but used only third line in the UK.[15] Failing that, the only treatment is anaesthesia in intensive care.[12][16] Phenobarbital is the first line choice for the treatment of neonatal seizures.[4][17][18] Concerns that neonatal seizures in themselves could be harmful make most physicians treat them aggressively. There is, however, no reliable evidence to support this approach.[19] Side effectsSedation and hypnosis are the principal side effects of phenobarbital. Central nervous system effects like dizziness, nystagmus and ataxia are also common. In elderly patients, it may cause excitement and confusion while in children, it may result in paradoxical hyperactivity. ContraindicationsAcute intermittent porphyria, oversensitivity for barbiturates, prior dependence on barbiturates, severe respiratory insufficiency and hyperkinesia in children. Overdose
Phenobarbital causes a "depression" of the body's systems, mainly the central and peripheral nervous systems; thus, the main characteristic of phenobarbital overdose is a "slowing" of bodily functions, including decreased consciousness (even coma), bradycardia, bradypnea, hypothermia, and hypotension (in massive overdoses). Overdose may also lead to pulmonary edema and acute renal failure as a result of shock. The electroencephalogram of a person with phenobarbital overdose may show a marked decrease in electrical activity, to the point of mimicking brain death. This is due to profound depression of the central nervous system, and is usually reversible.[20] Treatment of phenobarbital overdose is supportive, and consists mainly in the maintenance of airway patency (through endotracheal intubation and mechanical ventilation), correction of bradycardia and hypotension (with intravenous fluids and vasopressors, if necessary) and removal of as much drug as possible from the body. Depending on how much time has elapsed since ingestion of the drug, this may be accomplished through gastric lavage (stomach pumping) or use of activated charcoal. Hemodialysis is effective in removing phenobarbital from the body, and may reduce its half-life by up to 90%.[20] There is no specific antidote for barbiturate poisoning. PharmacokineticsPhenobarbital has an oral bioavailability of approximately 90%. Peak plasma concentrations are reached 8 to 12 hours after oral administration. It is one of the longest-acting barbiturates available – it remains in the body for a very long time (half-life of 2 to 7 days) and has very low protein binding (20 to 45%). Phenobarbital is metabolized by the liver, mainly through hydroxylation and glucuronidation, and induces most isozymes of the cytochrome P450 system. Cytochrome P450 2B6 System is more specifically induced by Phenobarbital. It is excreted primarily by the kidneys. Veterinary usesPhenobarbital is one of the initial drugs of choice to treat epilepsy in dogs, and is the initial drug of choice to treat epilepsy in cats.[21] It may also be used to treat seizures in horses when benzodiazepine treatment has failed or is contraindicated.[22]
Illicit UseThe High Incident Bandits used phenobarbital prior to committing the North Hollywood Bank of America robbery.[citation needed] Phenobarbital was mixed with vodka and consumed by the Heaven's Gate Cult members to commit suicide on March 26, 1997.[citation needed] Activist Abbie Hoffman committed suicide by consuming 150 phenobarbital pills on April 12, 1989.[citation needed] References
Categories: Barbiturates | Hypnotics | Anticonvulsants |
|||||||||||||||||||||||||||||||||||||||||||||||||||||
| This article is licensed under the GNU Free Documentation License. It uses material from the Wikipedia article "Phenobarbital". A list of authors is available in Wikipedia. | |||||||||||||||||||||||||||||||||||||||||||||||||||||